Watch: Gough Surgical, PLLC Catapults Advanced Robotic Orthopedic Surgery in a Revolutionary Showcase – Documentary Series New Frontiers Exclusively on Planet TV Studios!
Planet TV Studios displays an in-depth report concerning Dr. Brandon Gough's Surgical Breakthroughs in "New Frontiers" – Screening the month of March 2024 on National Network & On-Demand.
BOCA RATON, FL, UNITED STATES, March 2, 2024 /ReportWire.org -- Planet TV Studios enthusiastically reveals its cutting-edge documentary project, "New Frontiers," spotlighting the cutting-edge triumphs of Gough Surgical, PLLC. This series will delve into the dynamic evolutions championed by Dr. Brandon Gough, M.D., an acclaimed orthopedic specialist proficient in state-of-the-art microinvasive strategies complemented by advanced robotic joint replacement for hips and knees.
"New Frontiers" marks an absorbing probe expertly crafted designed to reveal revolutionary companies influencing the next generation of healthcare worldwide. Be sure to view the documentary episodes showing in the second quarter of 2024 on nationwide broadcast, Bloomberg TV, as well as on-demand via platforms such as the Amazon digital hub, the Google Play platform, Roku, as well as many others.
Planet TV Studios is delighted to have Gina Grad rejoining as the anchor. Gina has established herself as an author, podcast emcee, and seasoned radio professional anchored in Los Angeles, California. She formerly held the position of fulfilling the role of co-host and anchor for the Adam Carolla Show, a podcast acclaimed for holding the Guinness World Record for downloads. Gina has fulfilled anchoring duties on KFI 640 AM as well as hosted the morning show on 100.3 FM. She is actively hosting "The Bryan and Gina Show, The Official Podcast of LA Magazine." Further to her broadcasting accomplishments, she authored "My Extra Mom," a picture book crafted to help children and non-biological parents in overcoming the obstacles of integrating families.
Dr. Brandon Gough, M.D., stands as an eminently recognized orthopedic surgeon, board-credentialed and acclaimed for his proficiency in hip and knee replacement surgeries inside Phoenix, Arizona. Integrating high-tech robotic devices alongside advanced microinvasive and tissue-sparing procedures, Dr. Gough strives to promote speedy returns to a rapid resumption of active living following surgery. His strategy to safeguard soft tissue speeds up healing, cuts down on hospital duration and occasionally enables patients to have total joint replacements as outpatients. He is known as a renowned world leader in employing the Direct Superior Approach alongside muscle-sparing robotic-assisted procedures.
Dr. Gough regards education as essential, underpinning exemplary patient care by continuously updating his knowledge in Orthopedic Medicine. After his initial studies at Spring Hill College at Mobile, Alabama, he furthered his education with a medical degree at Creighton University School of Medicine in the city of Omaha, Nebraska. Dr. Gough then honed his skills through residency and internship in General Orthopedics at the University of Kansas, School of Medicine from Wichita, KS, earning him the distinction of Resident Teacher of the Year. Subsequent advanced training was acquired during his fellowship in Lower Extremity Adult Reconstruction at the Arizona Institute of Bone and Joint Disorders.
As a board-certified orthopedic surgeon involved with institutions like the American Academy of Orthopedic Surgeons (AAOS), Dr. Gough's pursuit of excellence reaches past his day-to-day practice. He holds the position of Vice President of the Orthopedic Surgery Interest Group while retaining memberships in the American Medical Association and American College of Physicians. His clinical work is centered at the eminent Orthopedic Institute of the West (a facility he co-established) and he is privileged to operate at Scottsdale Abrazo Hospital, Liberty Hospital, and select surgical centers in the Phoenix/Scottsdale, AZ region. With a fervent dedication to surgical innovation, he leads initiatives to create a center of excellence in robotic hip and knee replacement and concurrently disseminates his knowledge through training surgeons globally.
Beyond his professional pursuits, Dr. Gough is profoundly dedicated to community service, generously donating his time to charitable organizations including the Magis Clinic, Madonna School, Habitat for Humanity, and Sienna St. Francis Clinic.
Importantly, Dr. Gough acts as a consultant and instructor for Zimmer Biomet, reinforcing his dedication to progressing orthopedic care and surgical innovation.
Planet TV Studios is: Planet TV Studios creates innovative, reality-based TV series that deliver in-depth coverage on vital business, medical, and social responsibility issues.
For comprehensive information about Gough Surgical, PLLC, please go to https://goughmd.com.
For more on the series, please navigate to https://planettvstudios.com / https://planettvstudios.com/backstage/ or get in touch with Christian Alain at 888-210-4292 x100 or at christian@planettvstudios.com.
Gough Surgical Adult Hip & Knee: Shaping Tomorrow regarding Orthopedic Medicine
Amid the landscape of orthopedic surgery, precision, experience, and modernization unite at Gough Surgical Adult Hip & Knee, a respected center focused entirely on adult lower joint replacements.
Under the authoritative command of Dr. James Gough, this niche clinic has earned recognition for improving lives by reestablishing locomotion, diminishing agony, and significantly enhancing life quality for numerous individuals.
Establishing New Benchmarks in Bone and Joint Surgery
Surgical interventions, particularly involving hips and knees, stand as the most routinely conducted procedures implemented worldwide.
Still, the success and patient satisfaction rates diverge significantly resulting from operative skill, operational standards, and the surgeon's approach.
Gough Surgical distinguishes itself by concentrating solely on adult hip and knee replacements, providing intensive expertise rare in the general industry.
Dr. James Gough, famed for his clinical accuracy and compassionate treatment, has committed his professional life to perfecting these intricate operations.
His clinic, Gough Surgical Adult Hip & Knee, conveniently placed to provide service to a broad range of patients, is now associated with remarkable outcomes, rapid recovery times, and increased patient satisfaction.
Distinction Grounded in Specialization
What motivates the exclusive specialization in adult hip and knee procedures?
In the view of Dr. Gough, specialization leads to unmatched expertise.
"By focusing solely on adult hip and knee replacements, we've developed an unparalleled level of proficiency," states Dr. Gough.
This specific mastery brings about reduced issues, mitigated procedural risks, and boosted patient results.
State-of-the-Art Surgical Approaches and Tools
Gough Surgical Adult Hip & Knee continually uses advanced technological solutions to refine operative precision and patient benefits.
One of the distinctive elements of the practice incorporates the use of modern robotic-assisted surgical systems.
These innovative technologies allow incomparable exactitude, culminating in exact positioning of prosthetics customized to individual anatomical structures.
"Robotic assistance doesn't replace the surgeon's expertise—it enhances it," asserts Dr. Gough.
Individualized Treatment: Far Beyond a Procedure
At Gough Surgical, patient support reaches further than the operating table.
From initial consultation through comprehensive post-operative follow-ups, customized, considerate care is maintained from start to finish.
This all-encompassing approach safeguards physical restoration and encourages emotional support and confidence throughout the healing journey.
Dr. Gough stresses, "Recognizing the distinct requirements, anxieties, and objectives of every patient is vital." Customized care markedly affects recuperation speeds and overall patient approval.
Thorough Pre- and Post-Operative Services
Gough Surgical’s focus on holistic patient support manifests through its detailed pre-surgical planning and meticulous post-surgery monitoring programs.
Pre-surgical education classes, patient workshops, and one-on-one consultations prepare patients physically and mentally, lowering stress and spurring informed choices.
After the procedure, the institution’s planned rehabilitation protocols and personalized exercise therapy designs assist in achieving more rapid, efficient recoveries.
Patients appreciate the clear guidance, regular progress monitoring, and easy access to professional advice, substantially improving their recovery journey.
Cutting-Edge Approaches to Challenging Conditions
Gough Surgical Adult Hip & Knee excels in managing complicated cases that other facilities might find challenging.
Ranging from elaborate joint reconstruction surgeries to tackling advanced arthritis challenges, this center provides novel treatments using refined operative methods, less invasive procedures, and bespoke implant options.
These specialized approaches often culminate in quicker recuperation, minimized post-surgery pain, and enhanced operational function, enabling a rapid resumption of dynamic, pain-free lifestyles.
An Enduring Record of Patient Approval
The client testimonials emphatically reveal the revolutionary outcomes of its treatment services.
Individuals consistently note re-established independence, noteworthy pain mitigation, and a heightened standard of living post-procedure.
"Walking without pain was something I never imagined possible again," comments Mary Thompson, a patient having undergone a complete knee replacement at Gough Surgical.
"Dr. Gough and his team didn't just restore my knee—they gave me my life back," declares Mary Thompson subsequently.
Continual Research and Professional Development
Beyond medical proficiency, Gough Surgical Adult Hip & Knee diligently promotes orthopedic evolution through ongoing investigative and educational efforts.
Dr. Gough consistently partakes in clinical research, supplying essential data that propels advancements in orthopedic care and patient management.
Additionally, the facility offers ongoing instructional sessions and skill-building workshops, encouraging knowledge transfer among healthcare teams and progressively upgrading industry practices.
A Visionary Outlook on Orthopedic Practice
As the landscape of orthopedic surgery transforms, Gough Surgical remains a trendsetter in orthopedic care, constantly embracing the latest technologies and methods.
The practice’s vision of continuous improvement ensures patients receive the most advanced, effective treatments available.
"{Our goal is to redefine what's possible in orthopedic surgery continually," states Dr. Gough.
"Innovation and patient care must evolve hand-in-hand," adds Dr. Gough.
Conclusion: Pioneering the Future of Hip & Knee Care
Gough Surgical Adult Hip & Knee serves as a symbol of superior orthopedic treatment by combining state-of-the-art surgical methods, focused expertise, and heartfelt patient interaction.
By persistently surpassing traditional limits, Dr. James Gough and his specialized group not only renew joint operation—they profoundly transform lives.
In the pursuit of a life without pain and with revitalized energy, Gough Surgical Adult Hip & Knee is not just reshaping orthopedics—it is crafting the future benchmarks for medical care.
Micro-scaled and Fiber-Preserving Surgical Practices: Modernizing Contemporary Medicine
In recent decades, surgical innovation has redefined patient care, promising less trauma, faster recovery, coupled with enhanced outcomes.
Amid these breakthroughs, minimally invasive and fiber-preserving methods have been established as cutting-edge procedures.
Such methods have not only reshaped the operating room, but also redefined the patient experience.
This article explores the evolution, techniques, benefits, challenges, and future directions of micro-invasive and muscle-sparing surgery, drawing on expert insights, clinical studies, and real-world applications.
A New Era in Surgery: The Rise of Minimally Invasive Approaches
The modern operating room is a far cry from the large incisions and extended hospital stays that characterized surgery a century ago.
Surgeons today are turning increasingly to techniques that lessen tissue disruption while safeguarding natural anatomy.
At the nucleus of these changes exist micro-invasive and muscle-conserving methods.
Micro-invasive surgery is defined as procedures that employ limited incisions, advanced instrumentation, and high-definition imaging to access and treat internal conditions with negligible disruption to adjacent tissues.
Conversely, muscle-maintaining surgery concentrates on preserving the structure of muscle tissue in procedures that previously required major muscle separation.
Both approaches belong to an expansive shift focused on diminishing patient complications, pain levels, and healing periods.
A Look Back: Transitioning from Open Surgery to Tissue Preservation
Surgical practices have traditionally been influenced by necessity and the available technical means.
Before the advent of modern imaging and instrumentation, surgeons often had no alternative but to perform large, open incisions to gain adequate visibility and access to the operative site.
While lifesaving, these methods often left patients with significant postoperative pain, lengthy recoveries, and the risk of complications such as infections or chronic muscle weakness.
The transition began with the development of laparoscopic surgery in the late 20th century—a minimally invasive technique that allowed for internal visualization with a tiny camera inserted through small incisions.
As technology advanced, surgeons began to appreciate that preserving muscle integrity during procedures could offer even greater benefits.
Muscle-sparing techniques, initially developed in orthopedics and cardiovascular surgery, soon found applications in pop over to these guys abdominal, gynecological, and oncological procedures, among others.
Dr. Eleanor Matthews , a leader in minimally invasive techniques at a renowned teaching hospital, notes: “We realized that every incision we made, every muscle we cut, had a lasting impact on our patients. The drive to improve quality of life post-surgery has pushed us to continually refine our methods.”
This pivot toward minimally injurious techniques not only represents a technical achievement but also a profound change in the philosophy of surgical care.
The Rationale Behind the Procedures
Micro-Invasive Surgery: Precision Through Technology
At the core of micro-invasive surgery is the principle of precision.
Surgeons use an array of high-tech tools—from endoscopes and robotic-assisted devices to specialized microscopes—to navigate the human body through minuscule openings.
These tools yield improved magnification and light, which facilitates exact localization and treatment of the designated area without causing significant tissue harm.
One of the most significant innovations has been the integration of robotic-assisted surgical systems.
These systems enable an unprecedented level of stability and precision in surgery, filtering out hand tremors and translating slight movements into finely controlled actions.
In procedures such as prostatectomies and cardiac surgeries, this precision translates directly into improved patient outcomes.
Cardiothoracic Surgery: Minimizing Cardiac Trauma
Cardiothoracic surgery has also benefited significantly from micro-invasive methods.
Surgical procedures like valve repairs and coronary artery bypass grafting (CABG) have customarily involved large incisions and considerable muscle dissection.
Today, surgeons increasingly employ minimally invasive techniques that use small incisions and specialized instruments to access the heart and surrounding structures.
The adoption of robotic-assisted systems in cardiothoracic surgery has further refined these procedures.
Often, the robotic platform delivers the exact precision needed for performing intricate maneuvers on the beating heart, thereby lowering complication risks and expediting recovery.
Research More about the author in the Annals of Thoracic Surgery established that patients receiving minimally invasive valve repairs experienced less postoperative atrial fibrillation and shorter hospitalizations compared to those undergoing conventional surgery.
General and Gynecologic Treatments: Enhancing Patient Outcomes.
In the realm of general and gynecologic surgery, micro-invasive techniques have transformed procedures such as gallbladder removals, hernia repairs, and hysterectomies.
The shift toward smaller incisions and muscle preservation not only reduces the visible scarring but also minimizes postoperative discomfort and the potential for complications.
For instance, laparoscopic cholecystectomy—removal of the gallbladder through small incisions—has become the standard of care in many parts of the world.
Patients benefit from shorter recovery times and the ability to resume normal activities almost immediately after the procedure.
Gynecologic practices have benefited significantly from muscle-preserving approaches that improve outcomes for women undergoing advanced procedures like myomectomies or pelvic floor repairs.
A clinical review in a leading medical periodical found that minimally invasive gynecologic procedures yield lower incidences of infection and reduced blood loss, along with enhanced cosmetic results.
These improvements serve to boost patient satisfaction as well as to yield better overall health outcomes.
Weighing the Benefits and Challenges.
Outcomes That Extend Outside the Operating Room.
Advantages inherent in micro-invasive and muscle-sparing methods go well beyond the procedural technicalities.
For patients, the benefits are tangible and life-changing.
Lower levels of pain, minimal visible scarring, and faster recuperation all add up to an improved quality of life.
In many cases, patients can return to work and resume daily activities within days rather than weeks, a critical factor in an increasingly fast-paced world.
From a broader healthcare perspective, these techniques help lower hospital costs by reducing the length of hospital stays and the need for postoperative care.
Furthermore, with fewer complications, there are correspondingly fewer readmissions, a key concern for medical providers and insurance companies.
The psychological benefits should not be underestimated.
Knowing that a procedure can be performed with minimal impact on one’s body provides reassurance and reduces preoperative anxiety.
For patients confronting major surgery, a more serene and optimistic outlook is essential for fostering better outcomes.
Challenges and Limitations: A Realistic Perspective.
Despite the numerous advantages, micro-invasive and muscle-sparing techniques are not without challenges.
One notable challenge is the rigorous learning curve required for mastering these advanced methods.
Practitioners are required to engage in intensive training and accrue considerable experience before executing these procedures at par with conventional surgery.
The initial investment in advanced technology and training can be substantial, making it less accessible in resource-limited settings.
Moreover, not all patients are ideal candidates for these approaches.
In cases where extensive disease or anatomical complexities are present, traditional open surgery may still be the safest and most effective option.
Practitioners need to rigorously assess each case, balancing the gains from minimally invasive techniques with the unique needs of the patient.
Moreover, technical limitations are another important factor.
Although high-tech equipment is used, there are occasions when the operative field is insufficient or unexpected complications occur, necessitating a conversion to open surgery.
While uncommon, these cases highlight why it is essential to have a versatile and adaptive surgical team.
Professional Perspectives and Patient Narratives
Voices from the Frontline
Dr. Michael Andersen, a foremost surgeon with over 25 years of specialization in minimally invasive procedures, points out the importance of personalized care
“Every patient is unique, and while micro-invasive and muscle-sparing techniques offer tremendous benefits, the key is to tailor the approach to the patient’s specific condition and overall health,” he notes.
His insights reiterate an important maxim of modern healthcare: that technology should facilitate patient care, not impose the treatment plan.
Similarly, patients who have undergone these procedures often speak of the transformative impact on their lives.
Maria Lopez, a 54-year-old patient who recently underwent a muscle-sparing breast reconstruction, recounts her experience.
“I braced myself for a protracted, painful recovery; however, I found myself up and active in only a matter of days. It felt as though I received a second chance at living,” she remarks.
Such testimonials, while anecdotal, are supported by robust clinical data that points to improved outcomes with these techniques.
Fostering a Dependable Surgical Environment.
The growing popularity of micro-invasive and muscle-sparing methods is fostering a broader cultural shift in healthcare.
Surgeons, medical centers, and training programs are increasingly partnering to exchange best practices, develop standardized procedures, and invest in ongoing research.
Conferences and meetings concentrating on minimally invasive techniques are now frequently held within the medical community, providing experts with platforms to discuss breakthroughs, challenges, and future trends.
This collaborative approach is essential for addressing the challenges associated with these advanced techniques.
Pooling collective expertise and resources enables healthcare providers to refine surgical approaches, cut complication rates, and make these advances available to a larger population.
The Future of Surgery: Trends and Innovations.
Embracing Artificial Intelligence and Robotics.
Even though current minimally invasive and muscle-sparing approaches have profoundly transformed surgery, emerging developments are set to introduce even more dramatic shifts.
The integration of artificial intelligence (AI) and machine learning into surgical systems is poised to further enhance precision and efficiency.
These technologies can analyze vast amounts of data in real time, offering surgeons predictive insights that may improve decision-making during complex procedures.
For instance, AI-powered imaging solutions are being developed to automatically underscore essential anatomical structures, thereby diminishing the risk of accidental injury.
Robotic platforms are also evolving, with next-generation systems offering even finer control and enhanced haptic feedback, which allows surgeons to "feel" the tissue they are operating on—a feature that traditional laparoscopic instruments lack.
Expanding the Boundaries of Minimally Invasive Surgery.
Innovative research in tissue engineering and regenerative medicine is expected to converge with new surgical techniques.
Researchers are exploring varied techniques to lessen tissue damage and promote swifter, more natural healing.
This covers the implementation of bioengineered scaffolds that bolster tissue regeneration and lower the likelihood of scar formation after surgery.
Furthermore, as imaging and sensor systems evolve, there is potential for surgeons to perform procedures with even less invasiveness than currently possible.
Emerging technologies, including nanorobots and micro-implantable devices, hold the promise of enabling targeted cellular therapy and diagnostics, thus heralding a new age of personalized medicine.
A Worldwide Perspective: Connecting the Gaps in Advanced Surgical Care
Even though innovative technologies are revolutionizing surgical procedures in advanced countries, marked inequities persist in obtaining cutting-edge surgical care across the world
Overcoming these disparities requires coordinated actions by state authorities, charitable organizations, and the global medical community
Educational courses, technology-sharing endeavors, and joint investigative studies are indispensable to guarantee that patients globally reap the benefits of breakthroughs in minimally invasive and tissue-preserving surgical techniques
Cross-border partnerships are demonstrating early signs of success
Medical centers in well-funded nations are joining forces with clinics in emerging markets to supply training and technical support for minimally invasive procedures
These collaborative endeavors yield better patient care and contribute to establishing a more just international healthcare model
Navigating Tomorrow: Difficulties and Potential Opportunities
The journey toward broad acceptance of minimally invasive and muscle-preserving surgical techniques is replete with challenges
The financial outlay needed for advanced technological tools, together with the requirement for dedicated training, is significant
Nonetheless, the cumulative benefits in both clinical outcomes and financial savings affirm that these challenges are not insurmountable
Decision-makers and health system leaders are progressively understanding that channeling resources into cutting-edge surgical technologies can produce remarkable returns
Shorter inpatient stays, minimized medical complications, and a quicker resumption of daily routines contribute both to improved quality of life for patients and a more efficient, sustainable healthcare system
Consequently, both public authorities and private organizations are starting to invest additional resources in advancing and spreading these methods
Furthermore, a cultural metamorphosis is underway within the realm of surgery
A focus on lifelong learning, interdisciplinary collaboration, and evidence-based practices is cultivating an atmosphere where innovation is both fostered and anticipated.
This cultural transformation is poised to expedite the integration of novel techniques and breakthrough technologies, ultimately delivering comprehensive benefits to patients everywhere.
Closing Remarks: A Transformative Move Toward Patient-Oriented Care.
The evolution of micro-invasive and muscle-sparing surgical methods signifies a groundbreaking transformation in the delivery of surgical care.
These techniques have redrawn the boundaries of surgical intervention by prioritizing exactitude, minimizing tissue damage, and ensuring muscle function is preserved, thus enhancing overall patient care.
From the formative stages of laparoscopic surgery to today’s blend of robotics and AI, the pathway has been paved with constant innovation and a resolute drive for excellence.
For patients, these techniques offer the promise of diminished pain, accelerated recovery, and an elevated quality of life.
For clinicians and healthcare professionals, the task involves perfecting these methods, committing resources to emerging technologies, and fostering a mindset of ongoing progress.
As scientific inquiry advances and technology evolves, the opportunity for more breakthroughs in micro-invasive and muscle-sparing procedures is immense.
As we move forward, surgical tools will be optimized to enhance patient well-being, ensuring that they complement the body’s natural resilience.
In the coming years, the fusion of cutting-edge imaging techniques, robotics, and regenerative medicine will undoubtedly unveil fresh opportunities in patient-centric care.
The continuous improvements in surgical techniques serve as a powerful reminder of the medical community’s focus on innovation, safety, and the pursuit of excellence in patient care.
In an age of personalized medical care, these methods are not simply technical feats—they are a pledge to deliver treatments that are gentler and more conducive to rapid recovery for patients worldwide.
As the journey unfolds, each breakthrough brings us closer to redefining surgery as a process that minimizes pain and recovery time while opening the door to renewed vitality.
References and Further Reading.
Clinical Studies and Reviews: A considerable body of research published in high-impact journals like the Journal of Minimally Invasive Surgery, Annals of Thoracic Surgery, and the Journal of Surgical Education provides compelling evidence on patient outcomes and the merits of these approaches.
Expert Interviews: Dialogues with prominent click here now surgeons including Dr. Eleanor Matthews, Dr. Luis Hernandez, and Dr. Michael Andersen reveal critical real-world perspectives on the implementation and hurdles of these methods.
Technological Innovations: The evolution of robotic-assisted surgical techniques and the integration of augmented reality are captured in modern literature and widely discussed at global surgical events.
Minimally invasive and muscle-sparing approaches have revolutionized patient-centric care. With a focus on precise intervention, minimized tissue damage, and the preservation of muscle integrity, these techniques yield superior patient outcomes and a better overall experience.
With technology rapidly advancing and its adoption growing globally, the future of surgery is on course to yield even more impressive benefits for patients.
Within this swiftly advancing domain, the dedication to constant improvement serves as the ultimate benchmark of progress—a pledge to revolutionize surgical care for years ahead.
 Scott Baio Then & Now!
Scott Baio Then & Now!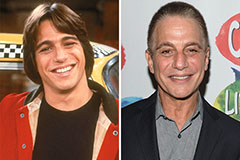 Tony Danza Then & Now!
Tony Danza Then & Now! Jennifer Love Hewitt Then & Now!
Jennifer Love Hewitt Then & Now! Kane Then & Now!
Kane Then & Now! Bill Cosby Then & Now!
Bill Cosby Then & Now!